CAN YOUR BODY FIGHT CANCER ON ITS OWN?
The history of medicine is a fascinating story of trial and error, with those trials often conducted on human beings. In the 19th century, there was no FDA, and that’s how immunotherapy happened to be discovered by a bone surgeon.
Although we now know that some streptococcus strains are part of the normal flora of the nose and throat, we knew far earlier that streptococcus bacteria could cause rheumatic heart disease, pneumonia, and pharyngitis. In the 19th century, injecting strep into a patient as treatment would have been unheard of.
But in 1891 when Dr. William B. Coley was just beginning his practice as a bone surgeon, he had a patient with inoperable cancer. Rather than just wait for the patient to die because he knew not to operate, he decided to test his theory that if he injected the patient with streptococcal organisms, the resulting infection would shrink the tumor as a side effect. It did, in what was probably the first instance of immunotherapy. The patient happened to be a friend of John D. Rockefeller, so Coley went on to run the Bone Tumor Clinic at Memorial Hospital in New York.
For forty years, he continued to inject more than 1000 patients with the bacterial products that became known as Coley’s Toxins. He had results with soft tissue sarcomas and bone cancers that were so good many other doctors didn’t believe them.
Parke Davis made the vaccine for him until 1963, when the thalidomide scandal brought greater regulation to the pharmaceutical industry and Coley’s Toxins were re-classified as a new drug that had to be used only in clinical trials. By then, both chemotherapy and radiation therapy had invented, so Coley’s vaccine, although based on correct first principles, gradually disappeared as a therapy.
Until, that is, the science of immunology experienced another growth spurt, albeit in a different direction. That growth was made possible by the discovery of T-cells in 1959 followed quickly by the concept of immune system surveillance — the idea that we have these T-cells in our lymphatic system whose functions are to watch out for foreign bodies and take up arms against them.
But even after we realized that the lymph system had something to do with fighting disease, doctors still disagreed about whether it was effective in tumor based diseases like cancer. First we had to go further in learning how antigens, molecules that can produce an immune response, produce antibodies, the actual disease fighting proteins.
Antigens are foreign bodies like bacteria, viruses and fungi that can cause disease. They can also be substances like allergens. The body has to recognize these foreign bodies as causes of disease in order to stimulate the immune response.
The antigens wake up certain helper cells called T-cells, Once these cells are activated, they begin to divide rapidly, forming an army to fight disease. But they need two different signals to activate, and that activation must be targeted to the correct molecular pathways to fight each specific cancer.
So far, scientists have been able to harness T-cells for a melanoma vaccine that has worked in a subset of patients. In another trial, gene transfer technology repurposes T cells to target them toward specific antigens present in lung cancer.
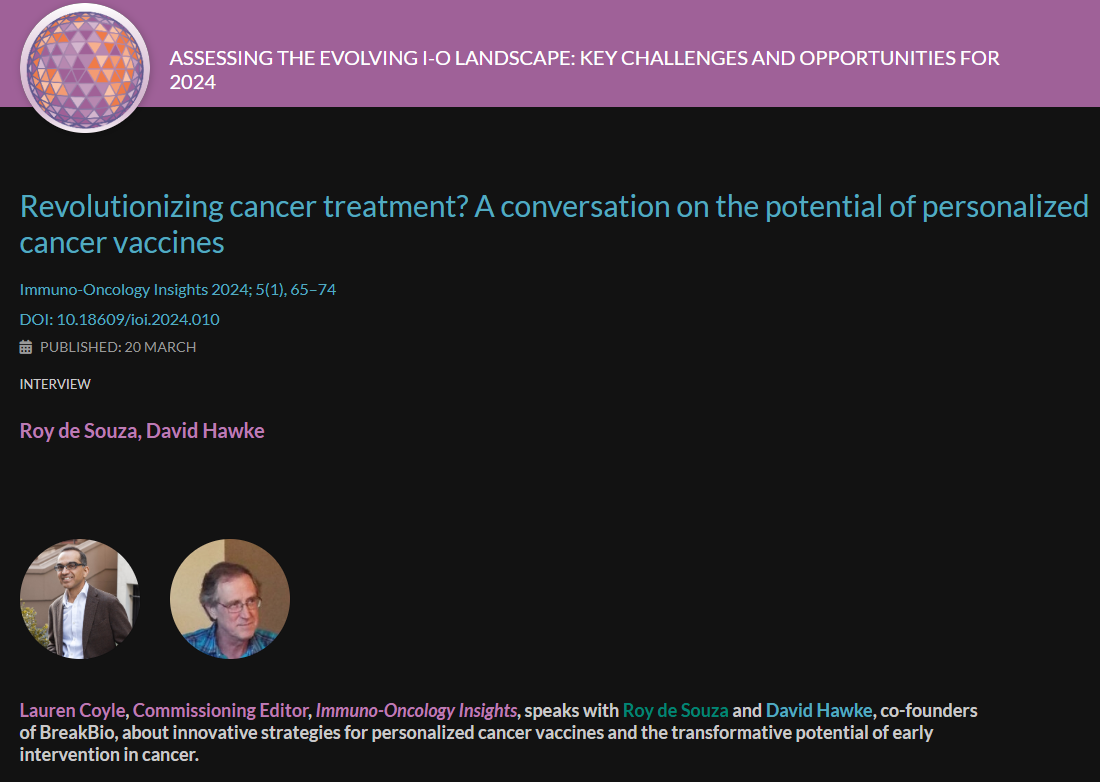
The idea of cancer vaccines is an exciting new frontier in both treatment and therapy. It’s the one we’re studying as we try to help advance the field.